Hair Transplant Clinic
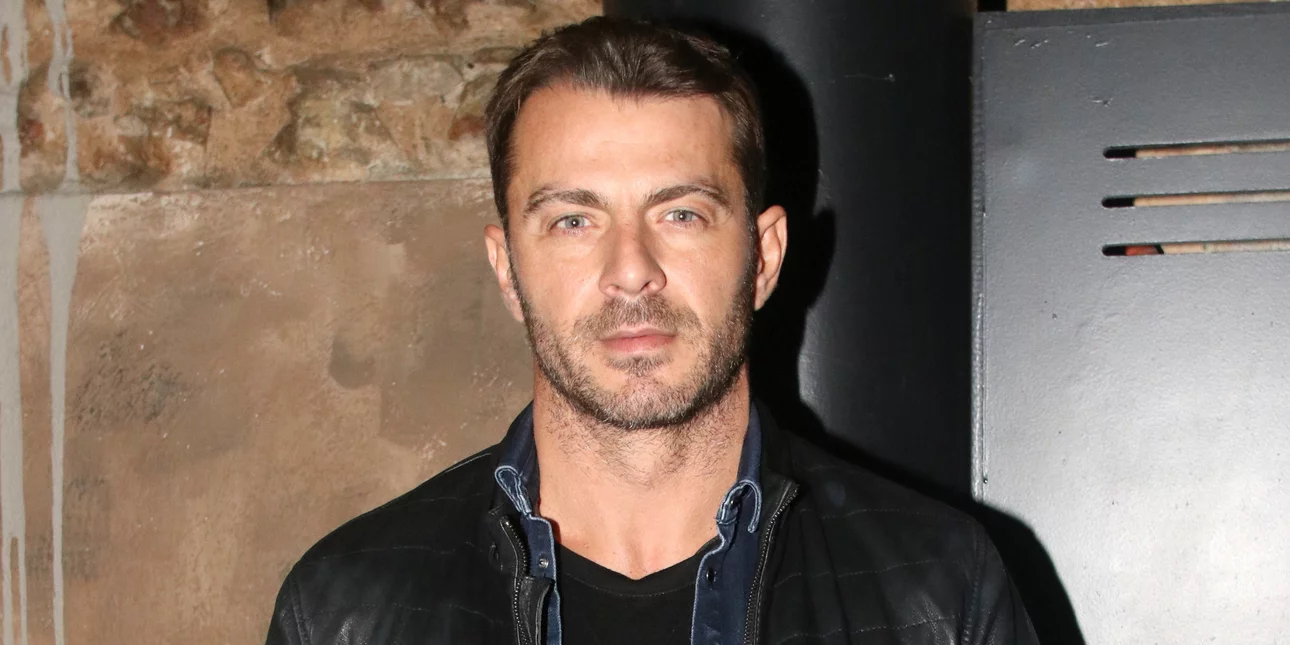
Ioannis Papangelopoulos MD, PhD
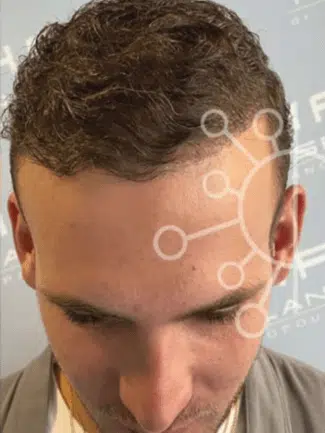
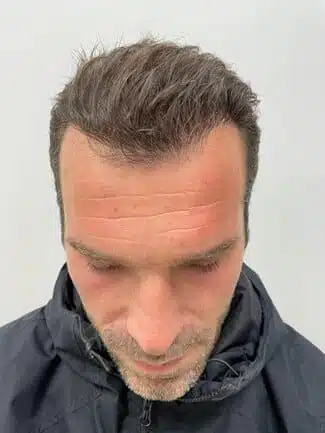
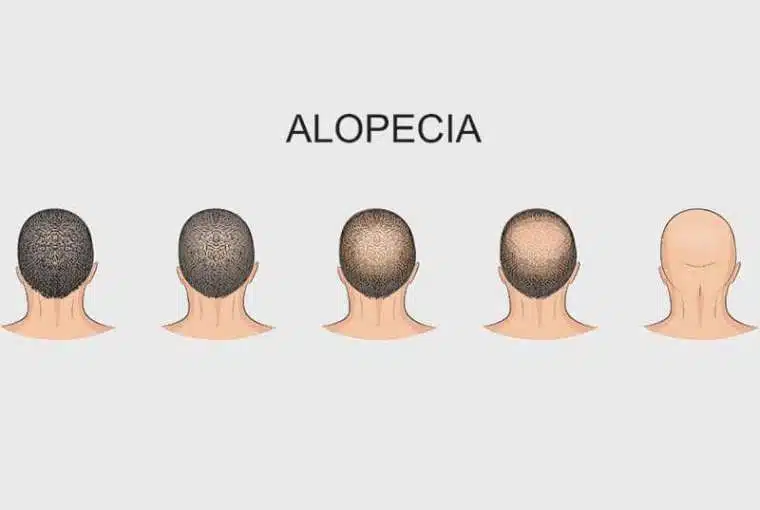
The hair transplant surgery is performed by Dermatologist-Dermatosurgeon Ioannis Papangelopoulos MD, PhD, and his team, using the innovative techniques of Hair Follicular Unit Transplantation.
-
1
Head of Hair Transplant Department at YGEIA Hospital
-
2
Dermatologist – Dermatosurgeon
-
3
Doctor of Medicine, University of Athens